Infectious disease detection and prevention
Learn more about how to detect and help prevent many infectious diseases
June 6, 2025

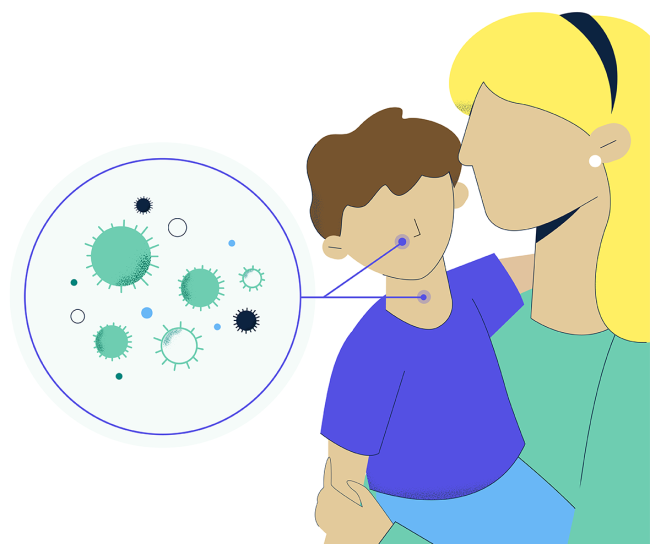
Infectious diseases are illnesses caused by pathogenic microorganisms such as bacteria, viruses, fungi and parasites that can spread directly or indirectly from one person to another. These diseases can range from mild to severe and can affect various bodily systems, potentially leading to significant health complications and, in some cases, death.
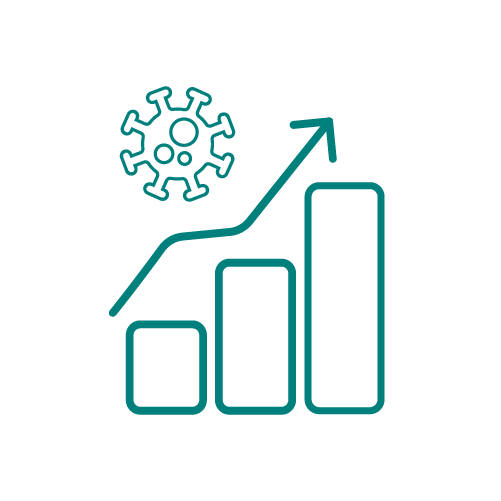
Vaccination is one way we can help protect against certain infectious diseases. However, in recent years, vaccination rates have been declining, which has contributed to outbreaks of some infectious diseases.
Outbreaks like these are a worrying sign of a heightened risk for the spread of vaccine-preventable diseases.
Information about certain infectious diseases
Hepatitis A | Hepatitis B | Measles | Mumps I Rotavirus I I Rubella
Hepatitis A
Hepatitis A is a disease of the liver caused by the hepatitis A virus, which spreads when someone ingests the virus, usually through person-to-person contact or by consuming contaminated food or drink. Those infected may feel sick for a few weeks or several months.
Signs and symptoms of hepatitis A
- Dark urine or clay-colored stools
- Feeling tired
- Diarrhea
- Fever
- Joint pain
- Loss of appetite
- Nausea
- Yellow skin or eyes (jaundice)
Potential risks and complications
In rare cases, hepatitis A can cause liver failure and death.
Hepatitis B
Hepatitis B is a disease of the liver that’s transmitted when blood, semen or another body fluid from a person infected with hepatitis B virus enters the body of someone who in uninfected (e.g., during sexual contact or childbirth). The disease can range from a mild, acute illness lasting a few weeks to a serious long-term, chronic infection.

Signs and symptoms of hepatitis B
- Dark urine or clay-colored stools
- Feeling tired
- Fever
- Joint pain
- Nausea, stomach pain or vomiting
- Yellow skin or eyes (jaundice)
Potential risks and complications
Approximately 15%-25% of people with chronic infection develop chronic liver disease, including cirrhosis, liver failure or liver cancer.
About 9 in 10 infants infected with hepatitis B ultimately develop a chronic infection, with the risk of chronic infection decreasing as the child gets older.
Measles
Measles is highly contagious and can cause serious health complications, especially in children younger than 5 years old. The disease spreads through the air when an infected person coughs or sneezes, with symptoms appearing seven to 14 days after contact with the virus.

Signs and symptoms of measles
- Fever
- Cough
- Runny nose
- Red, watery eyes
- Spots in mouth
- Rash
Potential risks and complications
Complications from measles include ear infections in about 1 in 10 children and diarrhea in fewer than 1 in 10 cases. Some children may suffer from severe complications, such as pneumonia (infection of the lungs) and encephalitis (infection of the brain).
Mumps
Mumps is caused by a virus that affects the salivary glands. The disease spreads through direct contact with saliva or respiratory droplets from the mouth, nose or throat. It can take two to four weeks for signs of infection to show.
Signs and symptoms of mumps
- Puffy cheeks and a tender, swollen jaw
- Fever
- Headache
- Muscle aches
- Tiredness
- Loss of appetite
Potential risks and complications
Although rare, mumps can cause serious complications, which include inflammation of the testicles (a condition known as orchitis).
Rotavirus
Rotavirus commonly spreads in families, hospitals and child care centers with symptoms usually starting about two days after a person is exposed to the virus. Some symptoms can last three to eight days.
Signs and symptoms of rotavirus
- Severe watery diarrhea
- Vomiting
- Fever
- Stomach pain
- Dehydration
- Loss of appetite
Potential risks and complications
Although usually self-limiting, severe illness can result in dehydration with shock leading to hospitalization or, on rare occasions, even death.
Rubella
Rubella, also known as German measles, spreads when an infected person coughs or sneezes. The disease is usually mild with few noticeable symptoms.
About 25 to 50% of people infected with rubella will not experience symptoms but will still be at risk of spreading the infection to others.

Signs and symptoms of rubella
- Fever
- Headache
- Mild pink eye (redness or swelling of the white of the eye)
- General discomfort
- Swollen and enlarged lymph nodes
- Cough
- Runny nose
Potential risks and complications
Rubella is especially dangerous to developing babies during pregnancy. If you’re pregnant and become infected with rubella, there’s an increased risk of having a miscarriage or the baby dying just after birth. The virus can also be passed on to the baby, who may develop congenital rubella syndrome, which includes birth defects such as heart problems, hearing and/or vision problems or developmental delays.
Understanding disease prevention
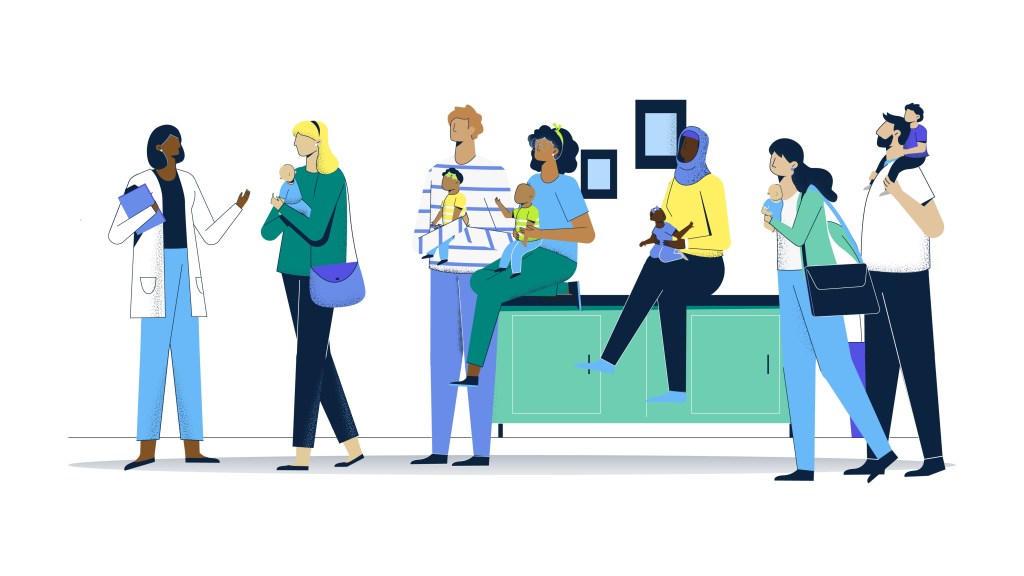
It’s important to learn about the potential risks of these diseases.
Talk to your health care provider about ways to help prevent infectious diseases including appropriate vaccines for you and your family.

Vaccines: Our history, our legacy
We’ve spent more than a century working to discover and develop vaccines.