Learn more about invasive pneumococcal disease and how infection spreads
Invasive pneumococcal disease can lead to a number of serious consequences in children
November 4, 2024

What is invasive pneumococcal disease?
Invasive pneumococcal disease (IPD) is an infection caused by a bacteria called Streptococcus pneumoniae. It can lead to a number of serious illnesses including pneumococcal bacteremia (an infection of the blood) and pneumococcal meningitis (an infection of the coverings of the brain and spinal cord).
Children under the age of 2 and those with certain underlying medical conditions are particularly vulnerable to invasive pneumococcal infection, according to the World Health Organization (WHO).
different types of S. pneumoniae, called serotypes, exist; however, a smaller number are responsible for most cases of IPD in children
of IPD cases occur in children under 2 years of age, on average, according to a 2019 paper by the WHO
How does pneumococcal infection spread?
Pneumococcal bacteria can spread anywhere, anytime through close contact with respiratory secretions, like those produced from coughing or sneezing. Children can carry the bacteria in their nose or throat without demonstrating signs of illness.
Pneumococcal infections are more common during winter and early spring, when respiratory diseases are more prevalent.
What you can ask your pediatrician about pneumococcal infection:
- Is my child at risk for invasive pneumococcal disease?
- How could invasive pneumococcal disease harm my child?
- What can I do to help reduce the risk of invasive pneumococcal disease for my child?
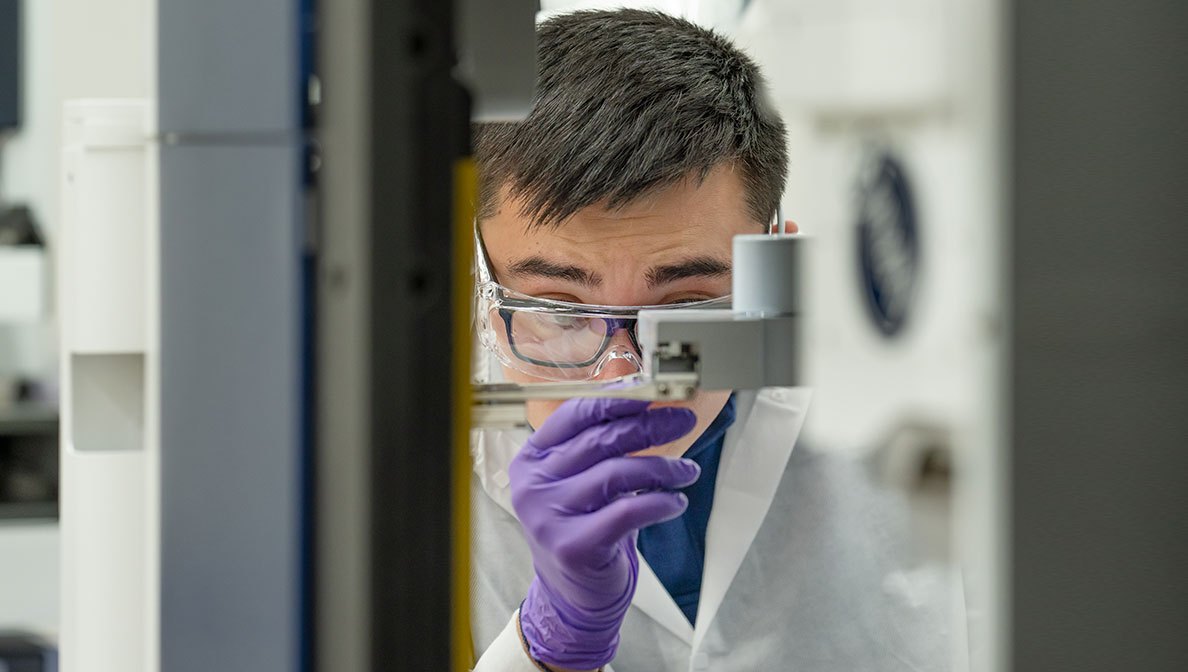
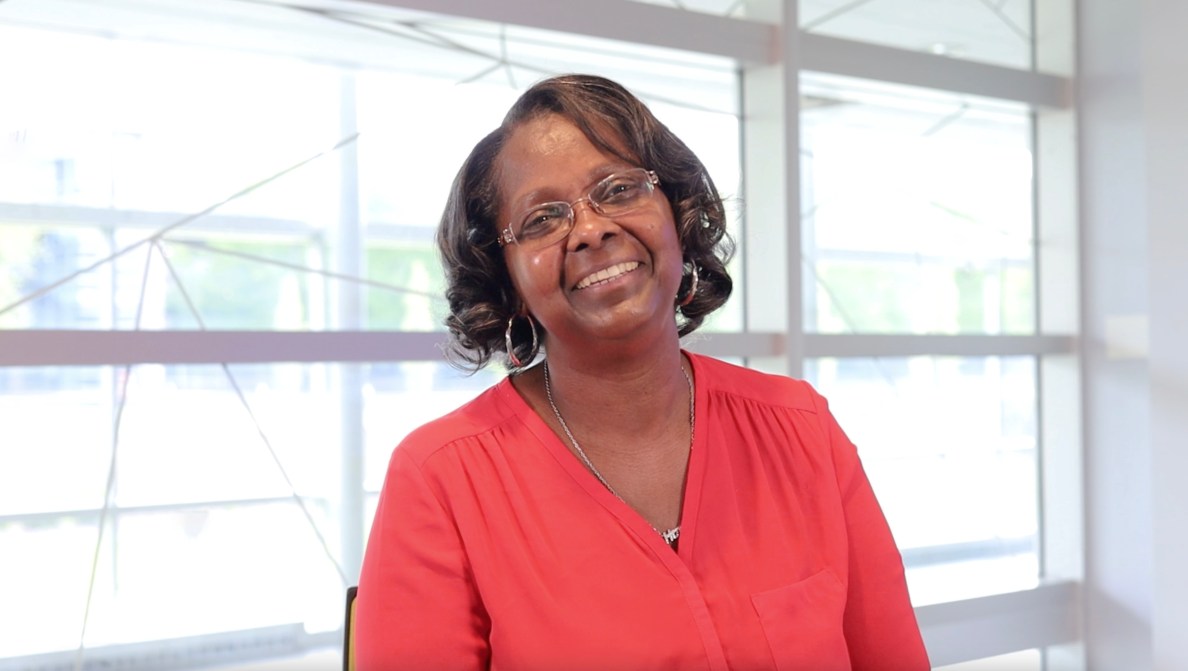
“There are steps people can take to be proactive about their family’s health. Parents should speak with their health care providers to learn more about invasive pneumococcal disease and the serious consequences it can cause.”
- Dr. Ulrike Buchwald, scientific associate vice president, clinical research